
When joints experience too much wear and tear, the cartilage diminishes and causes bones to rub together. Discomfort, pain, and sometimes immobility follow. However, total joint replacement in Kansas City provides long-lasting relief to reduce pain and enable patients to return to a normal life.
Our surgeons at Kansas City Orthopedic Alliance perform effective total joint replacement for patients in the Kansas City area and across the country. While surgery typically isn’t our first choice, we provide the best joint replacements possible when a patient requires an invasive procedure.
Why do people undergo a total joint replacement?
Most people undergo a total joint replacement due to osteoarthritis complications. Osteoarthritis comes from the wear and tear of the cartilage that surrounds joints. Cartilage plays an important role in how your joints move and feel by creating a layer of protection against direct joint connection. Therefore, a lack of cartilage can lead to inflammation and joint degeneration.
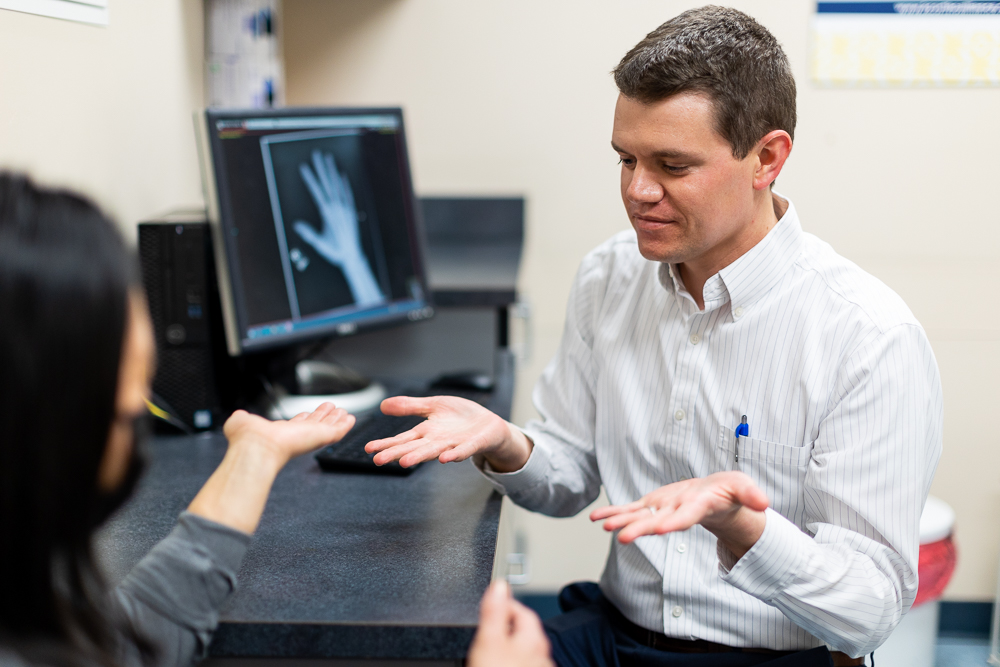
Diagnosing osteoarthritis requires an examination from an orthopedic physician, which may include tests such as X-rays and/or ultrasound. While we don’t recommend self diagnosing, you may have osteoarthritis if you experience the following symptoms:
- Joint stiffness
- Pain and swelling
- Loss of mobility
- Crunching sensation when moving joints
Some people are more prone to osteoarthritis than others. Factors that come into play include:
- Age
- Genetics
- Work injuries
- Physical activity (especially from athletes)
- Obesity
For many people, signs of osteoarthritis appear around their 50s, but they can emerge even earlier. For example, someone with an injury or a significant genetic predisposition could get an osteoarthritis diagnosis in their 40s.
Pain management for osteoarthritis in the shoulders, elbows, and ankles rarely involves physician intervention. However, procedures like shoulder replacements are still common. The more prominent issue derives from joints that affect walking such as the knees and hips. At that point, people often seek professional osteoarthritis treatments like total joint replacements to repair the problem.
An important thing to realize is that an osteoarthritis diagnosis doesn’t automatically mean you need surgery. In fact, orthopedic surgeons usually lean toward conservative measures before turning to surgery.
Osteoarthritis conservative treatment options

Since most people do not require surgery, conservative treatments can aid pain relief with the proper tools and expert guidance.
Combined with your test results, finding the right osteoarthritis treatment depends on the answers to the following questions:
- What caused your arthritis?
- How severe is your arthritis?
- Is the pain tolerable without help?
- What are your lifestyle goals?
- How has arthritis affected those goals?
From there, your provider will prescribe a treatment plan that may include:
Exercise
Despite popular belief, “resting” your joints isn’t always the best for your overall health. If your pain becomes too severe, then rest can definitely help; however, joints require movement. Synovial fluid lubricates joints to help them move across their various planes. Even small motions (you don’t have to perform high-intensity workouts!) increase synovial fluid, which in turn increases lubrication to limit pain. Additionally, synovial fluid boosts circulation throughout the entire body. That circulation supplies the nutrients and oxygen needed to promote joint health.
Medication
Over-the-counter NSAIDs (anti-inflammatory medications such as Advil) are a great way to alleviate flare up pain. While NSAIDs are typically safe to use, you should still speak with your physician to ensure they are the right option for you. Taking too many pills could lead to stomach irritation, ulcers, and kidney damage.
Injections
Injecting substances like cortisone directly into the affected joint can help with inflammation and pain. The effects typically last for 3 to 6 months before you would need another injection. Many people can manage arthritis pain through injections alone rather than a total joint replacement.
Regenerative Medicine
Proven by clinical trials, Regenerative options such as stem cell injections or platelet-rich plasma can help replace worn or damaged tissue. Although probably not suitable for severe arthritis (results are less conclusive in extreme cases), younger patients with mild-to-moderate arthritis may benefit from a regenerative medicine treatment.
How to know whether you need a total joint replacement in Kansas City
Assuming you are working with an orthopedic surgeon, he or she will help you determine whether you need a total joint replacement. Oftentimes, we recommend surgery when conservative measures alone don’t reduce pain and the osteoarthritis has led to joint degeneration.
You should never feel rushed to make the choice, especially because the decision for surgery relies on your timeline and goals. However, you also don’t want to suffer through pain longer than necessary or have to stop the physical activities you enjoy. As a general rule, we tell patients that if they can’t function, stay active, or maintain a healthy weight, then surgery may be the best option.
Many people believe it’s best to wait until later in life for a joint replacement. Unfortunately, this results in people suffering until their 70s. Instead, consider a replacement earlier (around your 60s) so you can enjoy the benefits of your total joint replacement longer.
How does a total joint replacement work?

A total joint replacement replaces the damaged arthritic joint with an artificial prosthesis. These are typically made of metal, plastic, or ceramic. The artificial joint effectively mimics the motion patterns of a healthy joint to improve your range of motion. Most commonly, people receive total joint replacements on their hips and knees.
After your joint replacement surgery, it is crucial for you to take care of your body. If you return to a sedentary lifestyle, you won’t be doing yourself much good. The best results come from dedication to your post-operative plan. This may include exercise, physical therapy, and generally remaining mobile.
Types of prosthetic implants for total joint replacements
During any kind of arthroplasty procedure, surgeons use an implant to replace the worn joint. The material your physician uses and the implant’s geometric shape depends on the patient and what he or she needs.
For example, in younger patients, we may use a material called oxinium. This material is a specialized metal that is smoother on a microscopic level compared to cobalt chrome. A smoother metal wears down plastic more slowly, which helps the new joint last longer and remain effective. For many people, this means they won’t have to come back for another replacement.
Two main determining factors of which type of material works best are:
- Age
- Activity level
Think of it this way: a 95-year-old patient won’t require a knee that lasts 30 years. So, choosing a more expensive material wouldn’t be necessary. On the other hand, an active person in their 50s or 60s may find more benefit in an oxinium implant despite the costs.
All of this is preplanned before surgery. Your physician should know which implant he or she will use before the procedure.
At Kansas City Orthopedic Alliance, we also have specialized orthopedic surgeons for the wrist, hands, foot, and ankle. Dr. Kneidel focuses on surgical procedures for the foot and ankle while Dr. Deardorff handles wrist and hand conditions. Therefore, whatever your need, KCOA has the expertise to guide you toward an effective treatment solution.
Robotic-assisted total joint replacement (specifically for knee replacement)
At KCOA, Dr. Abraham can go beyond traditional knee replacements through robotic technology. Robotic-assisted knee replacement utilizes mapping technology to increase the precision and accuracy of the surgery. We often remind our patients that robot assists in the surgery; they are not actually performing a knee replacement. Therefore, regardless of the technology, the results will only be as good as the surgeon’s expertise.
During a robotic-assisted knee replacement, Dr. Abraham puts reference points on the thigh and shin bone. This allows the computer to locate different body structures by using the triangulation and visual system. From there, Dr. Abraham takes a point probe with sensors and paints over the end of the bones. Sensors take that digital spatial information and convert it to a 3D picture on the computer.
As a result, Dr. Abraham can determine factors such as:
- Where to make the cuts in the bone
- How to position the implant
- How the implant affects the balance of the knee replacement
How do robotics compare to standard instruments?
Designed by engineers, standard instruments are based on the population average. The idea is very similar to a bell-shaped curve. The middle 80% represents the majority of patients, and that majority will fare pretty well after surgery. However, what about the 10% on either side? Traditional instruments only fit that 80%, not 100%. Sometimes, a surgeon won’t know whether you lie within that curve or outside of it until surgery.
Conversely, a computerized system allows a surgeon to digitally map your alignment before surgery. Even postoperatively, the system can check the implants to ensure the surgery has reestablished your normal alignment and laxity (the amount of looseness in the knee).
Recovery for total knee replacement
Whether you receive a robotic assisted or traditional knee replacement, the recovery process remains the same.
Overall recovery for a full knee replacement takes about three months. Since many people undergo an outpatient procedure, they return home the same day. However, outpatient procedures only work if you are healthy, motivated, and have strong support at home. After an outpatient procedure, you will typically begin walking and physical therapy the following day.
To help manage pain, your doctor may prescribe:
- Nerve blocks around the knee
- Injectable medications to avoid a lot of IV narcotics
- Oral narcotic pain medications
Physical therapy for a knee replacement usually consists of 2 to 3 sessions a week for about six weeks. However, this may vary from patient to patient. In some cases, therapy lasts longer based on how well a patient performs. Therefore, it is very important to remain in contact with your surgeon and physical therapist to ensure you are on the right path.
Going back to work will depend on the type of job you have. If you have a desk job or a job that is fairly inactive, you may be able to return after 2 to 3 weeks. However, if your job requires more strenuous activity and heavy labor, it could take up to three months.
Recovery for total hip replacement
Recovery for a total hip replacement will be slightly different. First, if you don’t have a strong support system at home, you’ll need to stay at a facility for 1 to 3 days after surgery. This allows you to begin the healing process with someone available to help.
What Happens During a Total Hip Replacement?
Those with support at home can leave after a day. Your doctor will prescribe pain medication to help you manage any discomfort. Remember, mobility is key. Therefore, you’ll want to start moving using a walker and physical therapy assistance (in house or at a facility).
Within a month or two, you should start feeling much better with minimal soreness. The great thing about the hip joint is that it tends to move better and become less stiff than the knees, which makes recovery much easier. Once the recovery process is complete, most people can expect their hip replacement to last for the rest of their lives. Both Dr. David Clymer as well as Dr. Abraham perform total hip replacements at KCOA.
Let KCOA provide the best total joint replacement in Kansas City
The core of our success lies in proper diagnosis. An appointment with one of our providers includes the highest quality technology to pinpoint a patient’s underlying musculoskeletal conditions. From there, we can better understand which treatment will work best for you.
For a thorough evaluation, call us at 913.319.7600 or schedule an appointment today.