Posterior tibial tendon dysfunction is the most common cause of adult acquired flatfoot deformity.
Anatomy and risk factors
The posterior tibial tendon is located on the inside of the ankle. It starts on the inside of the calf muscle and runs to attach to the bones on the inside of the foot. The posterior tibial tendon is responsible for holding the arch up and supporting the foot when walking. If this tendon is overused or torn, the tendon can become inflamed, which results in swelling and increased pain on the inside of the ankle and foot. An injury or high impact sports like tennis, basketball or soccer can cause the tendon to tear. Other risk factors include being over the age of 40, women, diabetes and obesity. Once the tendon becomes inflamed or torn, the tendon stops working properly and the arch collapses over time.

Symptoms
Along with pain and swelling on the inside of the ankle and foot people can also experience weakness, pain with activity such as running and walking and pain on the outside of the ankle. When the foot collapses the heel may shift outward, which puts more pressure on the outside of the ankle.
The common sign for posterior tibial tendon dysfunction is the “too many toes” sign. If you look at the heel from the back, you will see more than 1-2 toes. Patients are usually unable to perform a single limb heel rise. A patient cannot stand on one leg and come up on their toes to raise the heel. Patients may also have limited flexibility and limited range of motion of the ankle. The calf muscles may be tight, which limits how high the toes can point to the ceiling.
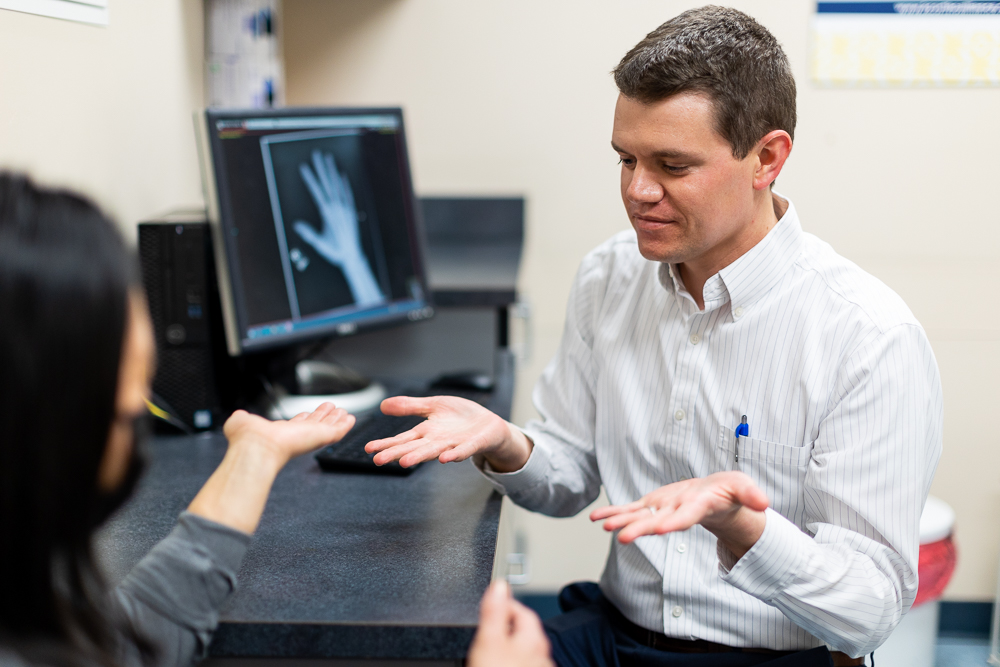
Testing
Standing x-rays are ordered to determine the severity of the flatfoot and whether arthritis is present in the foot or ankle. An MRI can be obtained to evaluate the posterior tibial tendon for any tears and evaluate for arthritis.
Treatment
Conservative treatments are tried first. Conservative treatments include rest, NSAIDs, ice, braces, orthotics, or physical therapy. An ankle airlift brace may be needed to help take the pressure off the tendon. A custom orthotic may be needed and is one of the most common conservative treatments. Steroid injections are not done for this issue.
Surgery
If pain still occurs after 3-6 months of conservative treatment, then surgery may be needed. Surgery is a big commitment as it requires 10 weeks of immobilization: 6 weeks of not walking on your foot in a cast, followed by 4 weeks walking on your foot in a boot. The first surgical option includes a tendon transfer and an osteotomy. An osteotomy is where the heel bone is cut, shifted and held together with a screw. During the tendon transfer the tendon that moves the little toes down is transferred to the posterior tibialis tendon. There is no loss of movement of the toes when this is performed.
If there is a lot of arthritis in the back of the foot and the foot is stiff, a tendon transfer and cutting the heel bone won’t work, so a surgery called a triple arthrodesis may be performed. In a triple arthrodesis, three joints are fused together to help decrease pain. During fusion surgery, the cartilage is removed, and the bones are held together with screws. Side to side motion is lost, but the up and down movement of the ankle is not affected. After surgery, a patient may not be able to participate in sports or run.